
Many foot diseases and conditions become more serious and common among the elderly. Some of these conditions include diabetic ulcers, ingrown toenails, fungus, arthritis, corns, and calluses. Unfortunately, it may be harder for older adults to take care of their own feet, but there are some precautions they can take in order to avoid any serious conditions.
Dry, cracked heels tend to be a common problem for older people. In order to avoid this, you should always keep your feet clean and well moisturized. Special feet moisturizers should be used as average lotions might not provide enough moisture for dry and cracked heels. Daily foot inspections are crucial for the elderly to detect any irregularities in their earliest stages. During the aging process, blood circulation tends to slow down causing older people to not feel their feet as well as they used to. This often results in foot problems going unnoticed.
Fungal and bacterial conditions thrive on elderly feet because older adults are less likely to keep their feet clean and dry; this makes it easier for bacteria to take hold in their dry, cracked skin. Elderly people should be sure to thoroughly dry their feet, especially in between the toes, after bathing. This will help them avoid developing any fungal infections. Additionally, clean cotton socks should be worn after the feet are dried.
Cutting toenails straight across will help prevent ingrown toenails. When toenails are cut too lose, the nail might break through the skin resulting in an ingrown nail. Clippers should be used to cut the nails in order to make the cut even.
Elderly people who have diabetes are at risk of developing serious foot problems that may lead to amputation. Ulcers that are left untreated can lead to gangrene. Dry and cracked feet, fungus, and untended cuts under the nails may also lead to infections.
Fortunately, Medicare covers many different types of services for foot care. Elderly people with any of these foot conditions should seek the help of a podiatrist and perform daily foot inspections in order to ensure that they have healthy feet.
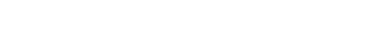
A bunion, medically known as hallux valgus, is a bony prominence that forms at the base of the big toe when the top of the toe shifts inward toward the others. This misalignment can lead to pain, swelling, redness, and difficulty wearing certain shoes. As a bunion progresses, the joint may become stiff, making simple movement uncomfortable. Some people also develop corns or calluses due to increased friction on the affected area. Contributing factors to bunion formation include inherited foot structure, flat feet, joint conditions such as rheumatoid arthritis, and aging. Although wearing tight or high-heeled shoes do not directly cause bunions, they can place additional stress on the foot, worsening symptoms. A podiatrist can assess the severity of a bunion and offer treatment to relieve pain and improve foot function. Options include padding, custom orthotics, or footwear modifications. In cases where pain is persistent or mobility is limited, surgery may be necessary to realign the toe. If you have a bunion that is interfering with daily activities, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options, which may include surgery.
If you are suffering from bunions, contact Dr. Robert Hope of Riverside Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
If you have any questions, please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.

Many people experience foot, toe, or ankle problems, either due to chronic health conditions like diabetes and arthritis, or from everyday factors such as wearing ill-fitting shoes or participating in strenuous activities like running. Podiatrists specialize in diagnosing and treating a wide range of foot, toe, and ankle conditions, providing relief through medication, specialized footwear recommendations, or surgery, when needed. Athletes frequently encounter injuries like sprains or shin splints, and a podiatrist can identify underlying issues and suggest preventive measures. Painful conditions like heel spurs, bunions, or ingrown toenails require professional intervention, as podiatrists can effectively manage these issues through targeted treatments or surgical correction. Diabetic patients benefit significantly from regular podiatric care, as it reduces the risk of severe complications, including infections that could lead to loss of limb. Conditions like persistent athlete’s foot, corns, or calluses also require expert care to achieve lasting relief. When you have foot, toe, or ankle problems, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Dr. Robert Hope from Riverside Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.

A swollen big toe can develop due to several underlying conditions, each leading to discomfort and pain. An ingrown toenail occurs when the edge of the toenail grows into the surrounding skin, causing inflammation and swelling. A toe fracture, which can happen due to trauma or accidents, may also result in swelling as the body reacts to the injury. Bunions are bony growths that develop on the joint at the base of the big toe and can cause the toe to swell and become misaligned. Gout, a type of arthritis caused by a buildup of uric acid crystals in the joint, is another common cause of a swollen big toe, often leading to intense pain and redness. If your big toe is swollen or you know you have any of the above foot conditions, it is suggested that you see a podiatrist who can offer you appropriate treatment solutions.
Toe pain can disrupt your daily activities. If you have any concerns, contact Dr. Robert Hope of Riverside Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
When to See a Podiatrist
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.

A neuroma is a thickening of nerve tissue caused by irritation, compression, or trauma. The most common type is Morton’s neuroma, which affects the nerve between the third and fourth toes. This condition develops when the nerve becomes inflamed due to repetitive stress, wearing tight footwear, or biomechanical issues, leading to pain, tingling, or a sensation of walking on a pebble. Over time, an untreated neuroma can worsen, causing chronic pain and permanent nerve damage. The affected nerve may continue to enlarge, making non-surgical treatments less effective. A podiatrist can provide relief through custom orthotics, footwear modifications, corticosteroid injections, or minimally invasive procedures. In severe cases, surgical removal of the neuroma may be necessary. If you think you have a foot neuroma, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and appropriate treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Robert Hope of Riverside Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.