 Anyone who is conscious about maintaining the health of their feet ought to be familiar with the important differences between mere dry skin on the feet and a case of athlete’s foot. The former condition does not always imply the existence of the latter. For example, if you have dry skin on your feet, you might notice a rough texture and even itching sensations. Sometimes dry skin is accompanied by cracked heels, also known as heel fissures. Athlete’s foot, on the other hand, is a kind of fungal infection that creates a red rash. Athlete’s foot can be contracted by walking around barefoot in highly trafficked public places, like locker rooms. Importantly, it is possible to have both dry skin and athlete’s foot at the same time. For more information about the difference between athlete’s foot and dry skin, contact a podiatrist today. This foot specialist will be able to answer any questions you might have.
Anyone who is conscious about maintaining the health of their feet ought to be familiar with the important differences between mere dry skin on the feet and a case of athlete’s foot. The former condition does not always imply the existence of the latter. For example, if you have dry skin on your feet, you might notice a rough texture and even itching sensations. Sometimes dry skin is accompanied by cracked heels, also known as heel fissures. Athlete’s foot, on the other hand, is a kind of fungal infection that creates a red rash. Athlete’s foot can be contracted by walking around barefoot in highly trafficked public places, like locker rooms. Importantly, it is possible to have both dry skin and athlete’s foot at the same time. For more information about the difference between athlete’s foot and dry skin, contact a podiatrist today. This foot specialist will be able to answer any questions you might have.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet, contact Dr. Robert Hope of Riverside Podiatry. Our doctor will assess your condition and provide you with quality treatment.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory-style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in Tuscaloosa, and Fayette, AL and Fayette, AL. We offer the newest diagnostic and treatment technologies for all your podiatric needs.
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing, or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder inside shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
 An open sore on the foot is known as a foot ulcer. It can be common among diabetic patients who have cuts on their feet, which they may not be aware of. A simple cut may develop into a foot ulcer as a result of neuropathy, which causes the inability to feel existing wounds, cuts, or scrapes on the feet. There are varying degrees of foot ulcers, which can range from a shallow wound that is on the surface to a deep wound involving the tendons and bones. Any type of wound on the foot needs prompt medical attention, and this may prevent a foot ulcer from developing. A wound on the foot is treated by cleaning out debris that may be inside of it. This is followed by tightly wrapping it with a bandage that can protect the foot, and it is beneficial to elevate it as often as possible. The more shallow the wound is, the greater the chances of a complete healing is possible. If you have a foot wound, please consult with a podiatrist who can offer the correct treatment methods for wound care.
An open sore on the foot is known as a foot ulcer. It can be common among diabetic patients who have cuts on their feet, which they may not be aware of. A simple cut may develop into a foot ulcer as a result of neuropathy, which causes the inability to feel existing wounds, cuts, or scrapes on the feet. There are varying degrees of foot ulcers, which can range from a shallow wound that is on the surface to a deep wound involving the tendons and bones. Any type of wound on the foot needs prompt medical attention, and this may prevent a foot ulcer from developing. A wound on the foot is treated by cleaning out debris that may be inside of it. This is followed by tightly wrapping it with a bandage that can protect the foot, and it is beneficial to elevate it as often as possible. The more shallow the wound is, the greater the chances of a complete healing is possible. If you have a foot wound, please consult with a podiatrist who can offer the correct treatment methods for wound care.
Wound care is an important part of dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Robert Hope of Riverside Podiatry. Our doctor will assess your condition and provide you with quality treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the utmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover it with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please feel free to contact our offices located in Tuscaloosa, and Fayette, AL and Fayette, AL. We offer the newest diagnostic and treatment technologies for all your podiatric needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
 Sesamoiditis is a foot condition that you might have heard of. It can occur in an individual when the two small sesamoid bones in the ball of the foot become inflamed. Interestingly, these two bones do not directly connect to any other bones. Rather, the sesamoid bones connect to tendons and muscles. When an individual has sesamoiditis, they may feel any number of symptoms. Most commonly, a patient might feel some kind of pain in the forefoot. This pain may be especially pronounced when putting weight on the feet. Additionally, a patient with sesamoiditis may unintentionally shift the weight of their body to the outside of their feet to avoid putting weight on the sesamoids when walking. These are just some of the many different symptoms that patients with sesamoiditis might demonstrate. Contact your podiatrist today for more information.
Sesamoiditis is a foot condition that you might have heard of. It can occur in an individual when the two small sesamoid bones in the ball of the foot become inflamed. Interestingly, these two bones do not directly connect to any other bones. Rather, the sesamoid bones connect to tendons and muscles. When an individual has sesamoiditis, they may feel any number of symptoms. Most commonly, a patient might feel some kind of pain in the forefoot. This pain may be especially pronounced when putting weight on the feet. Additionally, a patient with sesamoiditis may unintentionally shift the weight of their body to the outside of their feet to avoid putting weight on the sesamoids when walking. These are just some of the many different symptoms that patients with sesamoiditis might demonstrate. Contact your podiatrist today for more information.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Dr. Robert Hope of Riverside Podiatry. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
Treatment for sesamoiditis is non-invasive and simple. Podiatrists may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your podiatrist to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our offices located in Tuscaloosa, and Fayette, AL and Fayette, AL. We offer the newest diagnostic and treatment technologies for all your podiatric needs.
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscles. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high-arched feet, flat feet, or runners who run on the ball of their feet are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high-arched feet to relieve pressure off the bones. In some cases, the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore, you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
 There are different ways of fracturing a toe. A sudden increase in running or walking can produce a stress or hairline fracture, and can be uncomfortable. When a heavy object is dropped on it, or if it is jammed against a piece of furniture, it is considered to be more of a serious fracture, and there are noticeable symptoms that a break has occurred. These can include immediate bruising, and swelling, and the affected toe bone may protrude from the skin. If the break is very painful, a popping sound may be heard at the time of the injury. There is often a limited range of motion, and it can be difficult to walk. A proper diagnosis often consists of having an X-ray taken, and this is generally successful in determining how severe the break is. Many broken toes are treated by using the buddy taping method. This involves taping the broken toe to the toe next to it, which can provide the stability that is needed as the healing process occurs. If you have broken your toe, it is strongly suggested that you schedule an appointment with a podiatrist as quickly as possible, so the toe can heal correctly.
There are different ways of fracturing a toe. A sudden increase in running or walking can produce a stress or hairline fracture, and can be uncomfortable. When a heavy object is dropped on it, or if it is jammed against a piece of furniture, it is considered to be more of a serious fracture, and there are noticeable symptoms that a break has occurred. These can include immediate bruising, and swelling, and the affected toe bone may protrude from the skin. If the break is very painful, a popping sound may be heard at the time of the injury. There is often a limited range of motion, and it can be difficult to walk. A proper diagnosis often consists of having an X-ray taken, and this is generally successful in determining how severe the break is. Many broken toes are treated by using the buddy taping method. This involves taping the broken toe to the toe next to it, which can provide the stability that is needed as the healing process occurs. If you have broken your toe, it is strongly suggested that you schedule an appointment with a podiatrist as quickly as possible, so the toe can heal correctly.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Dr. Robert Hope of Riverside Podiatry. Our doctor will assess your condition and provide you with quality treatment.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions please feel free to contact our offices located in Tuscaloosa, and Fayette, AL and Fayette, AL. We offer the newest diagnostic and treatment technologies for all your podiatric needs.
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role in the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fracture is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms of a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
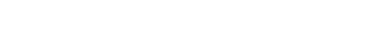
 One of the most common forms of heel pain that a podiatrist will encounter in patients is known as plantar fasciitis, a condition where the plantar fascia becomes inflamed. Many physical activities and sports may exacerbate this condition, particularly if it is high impact. However, in some respects, swimming may seem to be a helpful alternative for those with plantar fasciitis. Swimming is particularly low impact, enabling the athlete to burn calories while often not placing high pressure on the feet. It is important to note, however, that if someone has plantar fasciitis, it is possible that they still may experience pain when engaging in this activity. Someone with a particularly bad case of plantar fasciitis may feel pain if they try to push off of the wall with their feet when swimming. Schedule an appointment today with a podiatrist to learn more about plantar fasciitis.
One of the most common forms of heel pain that a podiatrist will encounter in patients is known as plantar fasciitis, a condition where the plantar fascia becomes inflamed. Many physical activities and sports may exacerbate this condition, particularly if it is high impact. However, in some respects, swimming may seem to be a helpful alternative for those with plantar fasciitis. Swimming is particularly low impact, enabling the athlete to burn calories while often not placing high pressure on the feet. It is important to note, however, that if someone has plantar fasciitis, it is possible that they still may experience pain when engaging in this activity. Someone with a particularly bad case of plantar fasciitis may feel pain if they try to push off of the wall with their feet when swimming. Schedule an appointment today with a podiatrist to learn more about plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Robert Hope of Riverside Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your podiatrist right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Tuscaloosa, and Fayette, AL and Fayette, AL. We offer the newest diagnostic and treatment technologies for all your podiatric needs.